The primary aim of Ayushman Bharat program is to achieve universal health coverage. National Health Policy 2017 envisage establishment of Ayushman Arogya Mandir to provide comprehensive primary health care that is universal, free and closer to the community.
To fulfill the aim, Ayushman Arogya Mandir Program was launched in 2018 and the first Ayushman Arogya Mandir was inaugurated by the Honorable Prime Minister at Jaangla, Bijapur Chhattisgarh on 14th April 2018.
Under the program, existing Sub- Health Centres (SHCs) & Primary Health Centres (PHCs) are being transformed as Ayushman Arogya Mandir and 1, 50,000 Ayushman Arogya Mandir will be operationalized by December 2022.
Click to view the real time update on number of Ayushman Arogya Mandir across the country.
Key components of Ayushman Arogya Mandir
The delivery of comprehensive primary health care through Ayushman Arogya Mandir is complex task as it requires a paradigm shift at all levels of health system. The operationalization of Ayushman Arogya Mandir requires several inputs.
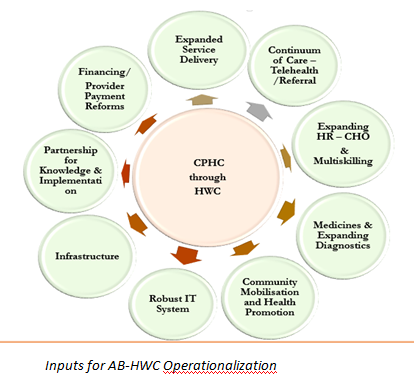
- Expanded Service delivery: Ayushman Arogya Mandir enable the expansion of the package of services that go beyond maternal and child health to include care for non -communicable diseases, palliative and rehabilitative care, Oral, Eye and ENT care, mental health and first level care for emergencies and trauma.
- Continuum of Care- Tele-health and referral:The delivery of comprehensive primary health care through Ayushman Arogya Mandir envisages a gatekeeping function, and a two-way referral system- that links to secondary and tertiary care and also follow up care. At all levels, teleconsultation are being done to improve referral advice, seek clarifications, and undertake virtual training including case management support by specialists.
- Expanding HR – CHO and multiskilling: A new cadre of worker Community Health Officer, trained in competencies of public health and primary health care has been posted at SHC-Ayushman Arogya Mandir. The Community Health Officer is expected to improve clinical management, continuum of care, dispensation of drugs and close follow up for those with chronic illness/patients discharged from health facilities . CHO leads the team of Multipurpose Workers, and ASHAs. All the service providers at Ayushman Arogya Mandir are being trained appropriately to deliver the expanded package of services to the community.
- Medicines and Expanding diagnostics: – Adequate availability of essential medicines and diagnostics enable medicine dispensation and necessary tests close to community. A total of 105 free and essential medicines at Ayushman Arogya Mandir-SHC and 171 medicines at Ayushman Arogya Mandir-PHC; and 14 diagnostic tests at Ayushman Arogya Mandir-SHC and 63 at Ayushman Arogya Mandir-PHCs are available for the community.
- Community Mobilization and Health Promotion – Health promotion at Ayushman Arogya Mandir is facilitated through engagement of community level collectives such as – VHSNCs, MAS and SHGs. Community mobilization, for action on social and environmental determinants, build on the accountability initiatives under NHM ensure that there is no denial of health care and universality and equity are respected
- Robust IT System- Ayushman Arogya Mandir team are equipped with IT equipment- Tablets at SCs and Laptop/ Desktop at PHC level to create electronic health record of the population covered by Ayushman Arogya Mandir. Developing a robust IT system will support Ayushman Arogya Mandir team to track patients for treatment adherence and follow up.
- Infrastructure – Ayushman Arogya Mandir are being upgraded and branded to provide sufficient space for expanded service delivery, for medicine dispensation, diagnostics organized, space for wellness related activities including the practice of yoga etc. with adequate spaces for display of communication material of health messages, including audio visual aids.
- Partnerships for knowledge and implementation- Partnerships with development partners and technical support agencies is being done to integrate Ayushman Arogya Mandir in their domain. These partnerships provide implementation support to the states, research and advocacy of Ayushman Arogya Mandir Program.
- Financing- provider payment reforms- Performance linked payment linked to the performance of Ayushman Arogya Mandir team have been introduced at Ayushman Arogya Mandir to foster team spirit. It is a mechanism to promote demand of health care in the community and deliver optimum and timely care close to the community.


